Hepatitis C
Hepatitis C
Viral hepatitis strikes thousands of Canadians resulting in short-term illness, chronic infections and even life-threatening consequences. One of the three most common forms of viral hepatitis is hepatitis C.
Hepatitis is a liver disease caused by the hepatitis C virus that attacks the liver. Many people who become infected with hepatitis C never feel sick and recover completely. Others get a brief, acute illness with fatigue and loss of appetite and their skin and eyes turn yellow (a condition called “jaundice”). If your body is not able to fight off the virus, you may develop chronic hepatitis which can lead to cirrhosis (liver scarring), liver failure and even liver cancer later in life. Like chronic hepatitis B, chronic hepatitis C is a “silent” disease because often no symptoms appear until your liver is severely damaged.
Could you have it?
Complete this hepatitis C risk assessment quiz and take it to your next doctor’s appointment. Let them know of your concern, and ask to be tested.
What are the symptoms?
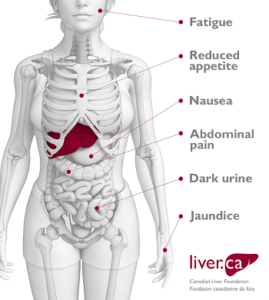 When you have just become infected with the hepatitis C virus, you may have no symptoms and may not even know you have been infected. This is the acute infection phase and can last from six to eight weeks, or longer. If you have symptoms, they are usually mild and may include fatigue, lethargy, nausea, reduced appetite, abdominal pain and jaundice.
When you have just become infected with the hepatitis C virus, you may have no symptoms and may not even know you have been infected. This is the acute infection phase and can last from six to eight weeks, or longer. If you have symptoms, they are usually mild and may include fatigue, lethargy, nausea, reduced appetite, abdominal pain and jaundice.
Over time, the virus may disappear on its own, and you are no longer infected. This happens to approximately 25 out of 100 hepatitis C-infected people. If the virus does not disappear after six months, your infection is chronic. This happens to approximately 75 out of 100 hepatitis C-infected people.
If your hepatitis C is chronic, in three out of four cases, you will have only very mild to moderate damage to your liver over time. However, in one out of four cases, chronic hepatitis C can lead to more serious problems including cirrhosis, liver failure and liver cancer over a period of 25 to 30 years.
You are more likely to develop cirrhosis if you drink alcohol, are obese, are male, became infected after age 40, have another type of liver disease or have another chronic infection, such as HIV or hepatitis B in addition to hepatitis C.
If I have no symptoms, how will I know if I have hepatitis C?
To determine whether or not you have hepatitis C, you will need to have blood tests. (see section entitled ‘Who should get tested?)
How do I get hepatitis C?
Hepatitis C is common worldwide. An estimated 170 million individuals worldwide including an estimated 250,000 in Canada are infected. Hepatitis C is spread through blood-to-blood contact, which means that to contract hepatitis C, blood infected with the hepatitis C virus must get into your bloodstream
You may risk exposure to hepatitis C by using injection drugs (even once), getting tattoos, piercings, pedicures, manicures or medical procedures with improperly sterilized equipment, sharing personal hygiene items with an infected person (e.g. razors, toothbrushes, nail clippers) or having had a blood transfusion or received blood products prior to July 1990.
Can I get hepatitis C more than once?
Although your body’s immune system makes antibodies to HCV, these antibodies do not protect you. The virus changes so quickly that it escapes your body’s defences. This means that you cannot have lifelong protection from hepatitis C. Also, no hepatitis C vaccine exists at this time. If you are treated for HCV and get rid of the virus, you can still be infected again. However, what you do, or do not do, can affect your level of risk for getting hepatitis C again.
How can I avoid getting hepatitis C?
There is no vaccine to protect you against hepatitis C. To avoid contracting hepatitis C, take the following precautions:
- Adopt safe sex practices;
- Avoid sharing personal hygiene items (e.g. razors, toothbrushes, nail clippers);
- Do not share needles; and
- If you decide to have a tattoo, piercing, manicure or pedicure, ensure that the facility uses single-use needles and inks and/or follows proper sterilization procedures.
Who is most at risk of contracting hepatitis C?
You have a high risk of contracting hepatitis C if you:
- use or have used injection drugs; even if it was just once or many years ago
- have received blood or blood products or an organ transplant before July 1990 in Canada
- have been in jail; or
- have been injected or scratched during vaccination, surgery, blood transfusion or a religious/ceremonial ritual in regions where hepatitis C is common.
You have a high moderate risk of contracting hepatitis C if you:
- have tattoos or body piercing;
- have multiple sexual partners;
- have a sexually transmitted infection (STI), including HIV or lymphogranuloma venereum (LGV);
- have experienced traumatic sex or rough sex or have used sex toys or fisting that can tear body tissue;
- have vaginal sex during menstruation;
- have received a kidney treatment (hemodialysis);
- have received an accidental injury from a needle or syringe;
- share personal items with a hepatitis C-infected person (e.g., razors, nail clippers, toothbrush);
- share cocaine (snorting) equipment;
- have another infectious disease (e.g., hepatitis B, HIV);
- were born to a hepatitis C infected mother; or
- have a sexual partner infected with hepatitis C.
Hepatitis C is NOT passed from person to person by:
- coughing, sneezing;
- touching or shaking hands with an infected person;
- sharing food, drinks, or eating utensils;
- using toilet seats;
- hugging or kissing;
- other casual contact;
- breastfeeding unless your nipples are cracked and bleeding; or
- oral sex, unless blood is present.
Testing
Ask your health care provider for a blood test to determine if you have the virus.
Why get tested for hepatitis C?
- An estimated 250,000 Canadians have Hepatitis C, but many don’t know it.
- Approximately 75% of people who are infected develop chronic infection and about 25% will clear their infection on their own.
- People with Hepatitis C often have no symptoms. Many infected people live for up to 20 or 30 years without feeling sick. When or if symptoms appear during the late stage of infection, they often reflect serious damage to the liver.
- Hepatitis C is a leading cause of cirrhosis, liver cancer and liver transplants.
- New treatments can cure Hepatitis C and prevent further liver damage and improve health outcomes.
Who should get tested for hepatitis C?
To determine whether or not you have hepatitis C, you will need to have blood tests. You should consider getting tested if:
- you were born between 1945 and 1975
- you are worried about having done something that could have put you at risk – even once or a long time ago (see sections entitled ‘How do I get hepatitis C?’ and ‘Who is most at risk’)
- you have signs or symptoms of having hepatitis C, such as nausea, fatigue, reduced appetite, jaundice, dark urine or abdominal pain
- you have resided in countries where hepatitis C is common (e.g., Egypt, southern Italy, India, Pakistan, Vietnam) and have been exposed to blood products, medical procedures, or vaccinations.
What to expect when getting tested for hepatitis C
The initial screening test is a blood test that looks for antibodies to the hepatitis C virus. This test is also called a hepatitis C antibody test (anti-HCV). These antibodies do not protect you against the infection.
- Ask your doctor when and how you will find out your results.
- Test results will take a few days to a few weeks to come back.
How to interpret what the hepatitis C antibody results mean?
If the test result is NON-REACTIVE/NEGATIVE
- A non-reactive or negative antibody test means that a person is not currently infected with the hepatitis C virus.
If the test result is REACTIVE/POSITIVE
- A reactive or positive antibody test means a person has been infected with the hepatitis C virus at some point in time. It does not tell you whether your infection is new, how long you have had it, or if the infection is still present.
- Most people who get infected with the hepatitis C virus, develop chronic (long-term) infection. However, about 25% of people who contract the virus, are able to get rid of or ‘clear’ the virus without treatment.
- Once people have been infected, they typically have antibodies to hepatitis C in their blood for life.
What to do if the hepatitis C antibody test is reactive
If the hepatitis C antibody test is reactive, a person needs an additional test to see if the hepatitis C virus (HCV RNA) is present in his or her blood HCV RNA test can tell if you still have the virus and how much of the virus is in your blood (viral load). The viral load does not relate to how severe your disease is.
If the Hepatitis C RNA test is:
- Negative—this means a person was infected with hepatitis C, but the virus has now been cleared from his or her body. This person is no longer infected.
- Positive—this means a person has Hepatitis C and is currently infected.
If a person has a reactive antibody test and a positive HCV RNA test, he or she needs to talk to a doctor experienced in treating hepatitis C to be monitored and to discuss treatment options.
HCV genotyping – this test identifies the type (or genotype) of the hepatitis C virus you have. There are six genotypes of HCV, numbered from 1 to 6, and you can be infected with more than one genotype at the same time. In Canada, genotype 1 is the most common.
Can hepatitis C be treated?
Yes, since 2010 enormous progress has been made in the treatment of chronic hepatitis C. New therapies called direct-acting antivirals (DAAs) are pills that act on the virus itself to eradicate it from the body, unlike older medicines like interferon injections which work by stimulating an immune response. These new treatments are very effective and can achieve cure rates of over 90%. In most situations now, there is no need for interferon, which was responsible for many of the side effects previously associated with HCV treatment. The new treatment combinations require shorter treatment durations (between 8 to 24 weeks), have reduced side effects and appear to be effective at all stages of the disease.
Because these new therapies are very new, they remain very expensive. As such, drug coverage from both government and private companies may require that your liver disease has progressed to a certain stage before they are willing to cover the cost of these drugs.
Your primary care physician may refer you to a specialist to determine whether you are eligible for treatment. A specialist will help you decide which drug therapy is best for you based on the severity of your liver disease, your virus genotype and whether or not you have been treated in the past.
If you are not presently eligible for treatment, it is important that you make sure to have your liver monitored at least once a year to follow the progression of the disease. You are strongly advised to have regular check-ups of your liver. Although liver failure and cancer can be the end results of this disease, your physician can identify liver changes long before this happens. Treating HCV drastically reduces these outcomes.
No alternative therapies which include herbal remedies, homeopathic medicines, and minerals have been proven safe and effective for treatment of hepatitis C. Be sure to tell your healthcare provider what medications and alternative therapies you are taking.
How can I cover medication costs?
New therapies called direct-acting antivirals (DAAs) are effective and can achieve cures of over 90%. Because these new therapies are very new, they remain very expensive. As such, drug coverage from both government and private companies may require that your liver disease has progressed to a certain stage before they are willing to cover the cost of these drugs.
Talk with your healthcare provider about financial support that may be available.
Below are useful resources when looking for financial assistance:
Private health insurance or drug plans
If you have private health insurance or a drug plan at work, you may be able to have the medication paid through your plan. Please consult your private health insurance or drug plan provider to see if your drug is covered.
Publicly funded plans
Each provincial and territorial government offers a drug benefit plan for eligible groups. Some are income-based universal programs. Most have specific programs for population groups that may require more enhanced coverage for high drug costs. These groups include seniors, recipients of social assistance, and individuals with diseases or conditions that are associated with high drug costs. For more details, please contact your provincial or territorial health care ministry, or click on the appropriate link below.
• Alberta (Prescription Drug Programs)
• British Columbia (Pharmacare)
• Manitoba (Pharmacare Program)
• New Brunswick (Prescription Drug Program)
• Newfoundland (Pharmaceutical Services)
• Northwest Territories (Drug coverage)
• Nova Scotia (Pharmacare)
• Nunavut (Drug coverage)
• Ontario (Drug Benefit Program)
• Prince Edward Island (Drug Cost Assistance Programs)
• Quebec (Prescription Drug Insurance)
• Saskatchewan (Drug Plan)
• Yukon (Insured Health)
Non-Insured Health Benefits for First Nations and Inuit
Health Canada’s Non-Insured Health Benefits (NIHB) Program provides coverage for a limited range of health care services when they are not insured elsewhere. For more information, please call 1-800-317-7878.
Pharmaceutical companies
Some pharmaceutical companies provide medications to patients who cannot afford them or who do not have government or private insurance under the Compassionate Use Programs. Each program has its own terms for eligibility. Please talk to your doctor to see if you are eligible for such a program.
Available Patient Assistance Programs for Hepatitis C treatment
• Abbvie Care 1 (844) 471-2273
– Holkira Pak (Ombivasvir/ paritaprevir/ ritonabir + dasabuvir)
– Maviret (Glecaprevir / pibrentasvir)
• Gilead Momentum HCV Support Program 1 (855) 447-7977
– SOVALDI (Sofosbuvir)
– EPCLUSA (Sofosbuvir / velpatasvir)
– HARVONI (Ledipasvir / sofosbuvir)
– VOSEVI (sofosbuvir / velpatasvir / voxilaprevir)
• MerckCare Hepatitis C Program 1 (866) 872-5773
– Zepatier (Grazoprevir / elbasvir)
Resources & Support
This website helps individuals assess if they are at risk for hepatitis C and provide a call to action to get screened and seek medical attention if required. This website is also for people looking for hepatitis C, sexual health, HIV or harm reduction services in Canada, with additional resources to support their journey to health and wellness. Search for services by location or by type of service.
Free Online Course about Hepatitis C
 In partnership with the BC Centre for Disease Control (BCCDC), we are pleased to offer you Hepatitis C: The Basics, a free online course that covers basic information about hepatitis C. It is intended for those living with hepatitis C, whether newly diagnosed or having lived with it for a number of years.
In partnership with the BC Centre for Disease Control (BCCDC), we are pleased to offer you Hepatitis C: The Basics, a free online course that covers basic information about hepatitis C. It is intended for those living with hepatitis C, whether newly diagnosed or having lived with it for a number of years.
This self-paced course includes videos and plain language narration.
To access the course:
1. Click here.
2. After a new window opens, click ‘Start Course’
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The National Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a Peer Supporter in your area, or would like to join the Peer Support Network, please fill out the Peer Support Network Sign-up Form
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.


