Biliary Atresia
Biliary Atresia
 Biliary atresia is a relatively rare disease that begins in early infancy and affects about one in every 10,000 to 20,000 infants. In biliary atresia, the bile duct that leads from the liver to the intestine becomes damaged preventing bile from leaving the liver.
Biliary atresia is a relatively rare disease that begins in early infancy and affects about one in every 10,000 to 20,000 infants. In biliary atresia, the bile duct that leads from the liver to the intestine becomes damaged preventing bile from leaving the liver.
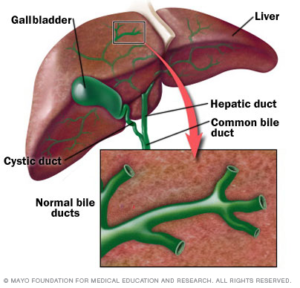
In the early stages the bile duct outside the liver is mainly affected, but in later stages, bile ducts inside the liver are also damaged. This can lead to a build-up of bile in the liver which can be harmful to the liver. Unless bile flow can be established, liver function is gradually lost and affected children rarely survive beyond two years of age.
 What is bile?
What is bile?
Bile is a yellow-green fluid made in the liver and stored in the gallbladder. It then flows through the common bile duct to the small intestine, where it helps with digestion and absorption of dietary fats and fat-soluble vitamins. Bile is also necessary for removing waste products from metabolism and toxins from the body.
Cause
The cause of biliary atresia is not known. It is not contagious, and it cannot be passed from one child to another. Biliary atresia is not believed to be related to genetics and is not connected to any aspect of prenatal care. Researchers currently believe that a complex process causes inflammation and blockage of the bile ducts.
Symptoms
Biliary atresia is usually diagnosed during the first two months of life. Common signs are:
- newborn jaundice that does not improve by two weeks of age, or jaundice that appears after two weeks of age
- dark urine and pale, clay-coloured stools
- enlarged liver or swollen abdomen
Diagnosis
Since the symptoms of biliary atresia may also be seen with other diseases, several tests are necessary to make a diagnosis. The following tests are performed:
- blood, urine and stool samples are analyzed
- the liver and bile ducts are examined with ultrasound
- a liver scan showing the liver and bile ducts is performed
- a liver biopsy is obtained
If the test results suggest biliary atresia, an operation is performed to examine the bile ducts and an x-ray is taken during the operation to determine whether the bile duct is blocked.
Treatment
It is essential that bile flow is established. Otherwise, the liver will suffer ongoing damage, resulting in liver failure. The most common treatment is an operation called the Kasai procedure (named for the surgeon who developed it, also referred to as portoenterostomy). In this operation, the damaged bile duct outside the liver is removed and replaced with a new drainage system made from a piece of the small intestine. This may partially or fully alleviate jaundice, but it will not reverse the liver damage that has already occurred or prevent any low-grade ongoing damage. The Kasai procedure is successful in one-third to one-half of all children and if jaundice is fully relieved, most children will grow and develop quite normally. However despite a successful Kasai procedure, cirrhosis, or scarring of the liver, generally continues to slowly occur.
What happens if the initial treatment fails?
 If the Kasai procedure fails to establish bile flow, the child will suffer ongoing health problems such as vitamin deficiencies, delayed development, inhibited growth, infections, a swollen abdomen, irritability, sleep disturbances, and bleeding into the gastrointestinal tract.
If the Kasai procedure fails to establish bile flow, the child will suffer ongoing health problems such as vitamin deficiencies, delayed development, inhibited growth, infections, a swollen abdomen, irritability, sleep disturbances, and bleeding into the gastrointestinal tract.
Vitamin deficiencies
Vitamins A, D, E and K are called fat-soluble vitamins because the body can only use them when they are bound to fat. If there is too little bile in the intestine for fat digestion, absorption of these vitamins becomes difficult. The baby may suffer from vitamin deficiency and may need to take extra vitamin supplements by mouth.
Delayed development and inhibited growth
If not enough bile reaches the intestine, the baby will not be able to digest the fat in his/her food. This makes it difficult to gain weight. A special baby formula can help maintain weight gain.
A child with biliary atresia may look quite jaundiced if bile flow has not been achieved. The liver may become enlarged, creating a ‘pot-bellied’ appearance. Frequent hospitalizations and long periods of feeling unwell may delay development of sitting, walking and other activities. Mental development, however, is usually normal.
Swollen abdomen
When the liver is not functioning properly babies often develop fluid in their abdomen. This condition is called ascites.
Most babies are not bothered by mild ascites, but if too much fluid builds up, it can become uncomfortable. Diuretic medications are often given to help children remove this fluid by increasing the amount of urine they produce.
Irritability and sleep disturbances
Babies often feel unwell as liver damage worsens because the liver is not able to remove the waste products of metabolism or toxins as easily from the body. As a result, infants become more irritable and over time they may also become difficult to settle. Sleep patterns can be affected and many children begin sleeping more during the day and are awake at night. To help treat and prevent a build-up of these toxins, medications can be given.
Bleeding into the gastrointestinal tract
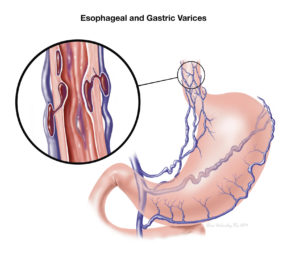
Liver damage may interfere with normal blood flow through the liver. As a result, blood from the intestine by-passes the liver, causing increased blood pressure in the veins of the stomach and esophagus. These veins may become enlarged and may begin to leak, causing internal bleeding.
Infections
Especially in children in whom the Kasai procedure relieves jaundice, infection can be a problem. Infections can develop in the new drainage tube. Symptoms of infection include fever, irritability and increasing jaundice. Infections are treated with antibiotics.
When is a liver transplant necessary?
When it proves difficult or impossible to achieve adequate bile flow and liver failure develops, liver transplantation is a final option. Replacing the liver in this way is successful in about 80-90 per cent of cases. The largest obstacle to the transplantation of all children with liver failure from biliary atresia is the lack of liver donors in this age group. For some children, living related donor (LRD) transplants may be an option.
What precautions should be taken?
No precautions are possible as biliary atresia occurs without warning, only in infants and is not passed from one person to another. Early intervention is the best course of action. If jaundice persists after two weeks of age or develops after two weeks of age, or clay-coloured stools are noticed, it is important to have the infant see a doctor.
What else can we learn about?
Identifying causes of biliary atresia and other liver diseases in children is the key research goal. The Canadian Liver Foundation supports educational programs and research into the causes, diagnoses, prevention and treatment of liver disease.
Support
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a Peer Supporter in your area, or would like to join the Peer Support Network, please fill out the Peer Support Network Sign-up Form.
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.



