Primary Biliary Cholangitis (formerly Primary Biliary Cirrhosis)
Primary Biliary Cholangitis
Formerly known as Primary biliary cirrhosis, PBC is a disease that affects predominantly women aged 40-60. Thanks to improvements in our ability to treat and manage PBC, less than 50 percent of patients progress to cirrhosis. Because of this fact and the issue of ‘cirrhosis’ often being connected solely to alcohol, PBC patients around the world pushed for a name change. Hepatologists agreed with the need to change the name to more accurately reflect the nature of the disease.
Primary biliary cirrhosis is now known as primary biliary cholangitis. It permits the continued use of the short form PBC while providing a more accurate description of the disease. This change has been endorsed by the Canadian Liver Foundation, the Canadian Association for the Study of the Liver (CASL) as well as PBC patient groups and professional associations of liver specialists worldwide.
What is Primary Biliary Cholangitis?
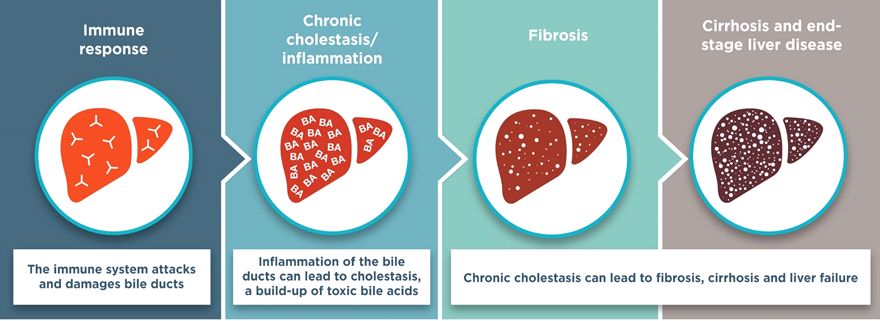
Primary biliary cholangitis, formerly known as primary biliary cirrhosis, is a chronic liver disease. When a person has PBC, the immune system attacks the liver causing slow, progressive damage to the bile ducts (small tubes through which bile flows out of the liver).
Bile is a yellow-green fluid produced by your liver to aid digestion. When the bile ducts are damaged, bile and other substances cannot be eliminated and accumulate in the liver. The retained substances are harmful to the liver and worsen the inflammation which leads to further damage. This can over time result in scarring of the liver. When there is a lot of scarring in the liver this is called cirrhosis.
The disease is called primary biliary cholangitis (PBC) because the immune system attacks the bile ducts inside the liver, which damages them. When immune cells surround and attack parts of the body, this is called inflammation. Inflammation of the bile ducts is called cholangitis. The medical term “primary” in this case means that there is no known reason for this damage to happen. Because the disease blocks or prevents the flow of bile, PBC is known as a “cholestatic” liver disease.
Who is at Risk?
PBC generally affects women between the ages of 40 and 60, but it has been diagnosed outside of this age range, as well as in men. Nine out of 10 people who get PBC are women. Although there is no evidence that PBC is inherited from mother to child, it is more common in the daughters of women with PBC.
Cause
The cause(s) of PBC remains unknown, but current evidence suggests that PBC occurs in genetically predisposed people after exposure to an undetermined environmental factor. It is important to note that PBC is not caused by alcohol consumption.
PBC is believed to be an autoimmune disease. In the case of PBC, your immune system which is designed to protect you against infections and cancer mistakes the bile duct cells as being not a normal part of the body and attacks them.
Something may trigger your body into making this mistake. Possible causes of this “trigger” could be an infection or some form of toxin exposure from the environment.
PBC usually develops and progresses slowly. Medication can slow its progression, especially if treatment begins early.
Could I Have It?
Many people with PBC have no symptoms. However, when they do, symptoms may vary and may be present in any combination and include:
- mild to disabling chronic fatigue
- mild to intense and unrelenting itching of the skin (often on palms or soles of the feet)
- gradual darkening of the skin
- small white bumps under the skin, usually around the eyes.
Other symptoms, not directly related to PBC, are also often reported by patients:
- dry membranes (nose, eyes, mouth, vagina)
- thyroid problems
- arthritis
- fingers and/or toes that change colour in the cold (Raynaud’s disease).
Importantly, many people with PBC never develop any symptoms related to the disease. Most commonly reported symptoms are fatigue and itching in any part of the body. Itching, also medically referred to as pruritus, may be the result of your liver’s inability to process bile.
If liver damage progresses in PBC, other symptoms may appear, which can affect other parts of the body outside of the liver. These symptoms include:
- enlarged abdomen from fluid accumulation (ascites)
- easy bruising or bleeding
- jaundice (yellowing of the skin and eyes)
- internal (gastrointestinal) bleeding
- bone pain or spontaneous fracture can also occur due to osteoporosis.
Diagnosis
Diagnosis of PBC is typically made with specific blood tests:
Most people with PBC have something in their blood called antimitochondrial antibody (AMA). An antibody is a protein made by your body’s immune system to attack an “invader”. The presence of AMA in your blood is an important sign that you have PBC.
- Increased levels of alkaline phosphatase (ALP), an enzyme released into the blood by damaged bile ducts.
- Increased levels of the immunoglobulin IgM.
- The liver enzymes alanine transaminase (ALT) and aspartate transaminase (AST) are also monitored by your doctor although these enzymes are a measure of inflammation relating primarily to liver cell damage/destruction, rather than bile duct cell damage.
In addition, your healthcare provider may request other tests:
- An abdominal ultrasound scan may be used to check the condition of the bile ducts, to make sure there is nothing else causing decreased bile flow out of the liver.
- A liver biopsy may be performed to see how serious your condition is. In this procedure, a small needle is inserted into the liver to take a sample of the tissue for analysis.
- A FibroScan® test (also called transient elastography), which is similar to an ultrasound test but gives information as to how stiff your liver is. The higher the stiffness (the number generated by the test), typically the more scarring there is in the liver.
PBC is a slow, progressive disease, which means that damage to the liver typically gets worse over a long period of time.
Treatment
PBC is a chronic liver disease. This means that PBC is a long-lasting condition that can currently be controlled in the majority of people, but not cured. The prognosis of PBC has improved over the last two decades due to earlier diagnosis and improved treatment. Early access to treatment can significantly delay progression of the disease. The outcome for PBC patients who are cholestatic and take treatment is better than for those who are not receiving treatment and can even be the same as people who do not have PBC.
- A medication called ursodeoxycholic acid (also called UDCA, URSO) mimics a naturally occurring bile acid. This medication can improve liver function and delay the development of fibrosis (scar tissue) in the liver, which in turn can delay or eliminate the potential for PBC to progress towards liver failure and/or liver transplantation.
- Vitamins A, D, E and K can be prescribed, usually when severe cholestasis and jaundice is present.
- Various medications may be prescribed by your doctor to help reduce itching. Some examples of these medications include cholestyramine, antihistamines or other medications.
- Complications of liver deterioration can often be controlled. As an example, a salt-restricted diet and medication (usually water pills) can be prescribed following accumulation of fluid in the abdomen.
A number of new medicines are currently being developed to treat PBC, typically to be added to UDCA therapy. Obeticholic acid (OCA), which is a man-made bile acid that acts to reduce liver inflammation and cholestasis, is available in Canada.
Liver transplantation may be recommended for eligible candidates if other treatments are no longer helpful, and liver damage and scarring has progressed to the point that the liver is no longer able to work properly. Liver transplantation works well for people with PBC, although it is possible to develop PBC in your new liver.
How do you know if your PBC treatment is working?

How can I pay for my medication?
Private health insurance or drug plans
If you have private health insurance or a drug plan at work, you may be able to have the medication paid through your plan. Please consult your private health insurance or drug plan provider to see if your drug is covered.
Publicly funded drug plans
Each province and territory has their own rules. Some provincial drug plans provide coverage for individuals 65 and older, or those on social assistance. Some provinces (e.g. Ontario) provide special support to low-income individuals. Please call your Provincial Ministry or Department of Health to get more information about the terms of the publicly funded drug plan in your province. (see links on page 13 of the “How To Health Guide”)
Quebec public drug program
In Quebec, everyone must be covered by prescription drug insurance either through private or publicly funded plans.
Each provincial and territorial government offers a drug benefit plan for eligible groups. Some are income-based universal programs. Most have specific programs for population groups that may require more enhanced coverage for high drug costs. These groups include seniors, recipients of social assistance, and individuals with diseases or conditions that are associated with high drug costs. For more details, please contact your provincial or territorial health care ministry, or click on the appropriate link below.
• Alberta(Prescription Drug Programs)
• British Columbia (Pharmacare)
• Manitoba (Pharmacare Program)
• New Brunswick (Prescription Drug Program)
• Newfoundland (Pharmaceutical Services)
• Northwest Territories (Drug coverage)
• Nova Scotia (Pharmacare)
• Nunavut (Drug coverage)
• Ontario (Drug Benefit Program)
• Prince Edward Island (Drug Cost Assistance Programs)
• Quebec (Prescription Drug Insurance)
• Saskatchewan (Drug Plan)
• Yukon (Insured Health)
Pharmaceutical companies
Some pharmaceutical companies provide medications to patients who cannot afford them or who do not have government or private insurance under the Compassionate Use Programs. Each program has its own terms for eligibility. Please talk to your doctor to see if you are eligible for such a program.
Available Patient Assistance Program for Primary Biliary Cholangitis treatment
• NAVIGATE Patient Support Program 1 (844) 628-4484
– OCALIVA (Obeticholic acid)
How do I take care of myself?
There are a number of treatments for the symptoms of PBC.
Itchy skin: Cholestyramine may be prescribed by your doctor to help ease itching. Cholestyramine is taken orally and works by preventing re-absorption of the chemicals (bile acids) that cause the itching. Sometimes rifampicin, naltrexone or sertraline may be prescribed by your doctor. In addition to medications, a skin moisturizer may be beneficial as itching is made worse by dry skin. As well, avoid taking hot baths and hot showers which may dry out your skin further.
Dry eyes and dry mouth may be relieved by artificial tears and saliva, lubricating gels and creams. Sugarless lozenges and gum may help with the dryness in your mouth. Good dental hygiene is very important. Biotène® products may also be helpful for dry mouth.
Diet: A healthy diet is important to liver health. Specific things to keep in mind include:
- Maintain a healthy caloric intake recommended for your age, gender and activity level.
- Eat from all four food groups, including fruits and vegetables, whole grains and cereals, milk products and meats and alternatives.
- Limit your intake of salty, sugary and fatty foods.
Alcohol can damage your liver. If you have a liver disease, you should avoid drinking alcohol.
Taking medication: Talk to your healthcare provider before taking any medicine or treatment, including over-the-counter supplements and herbal remedies. Many medicines may have unwanted side effects and interactions.
Dealing with fatigue: The cause of fatigue in PBC is unknown. It is important for your doctor to rule out other potential non-PBC -related causes of fatigue, including anemia and thyroid problems. If you feel tired and unable to carry out day-to-day tasks, you may find that some lifestyle changes can make a difference:
- Pace your activities.
- Try daily aerobic physical activities such as walking and swimming to help make you more fit without becoming exhausted.
- Adjust your hobbies and daily activities to more closely match your energy level.
Bone health: As we get older our bones often become thinner and more brittle. This is more common among women, especially after menopause. PBC may make this worse. You can help prevent this problem by doing plenty of weight-bearing exercises and eating food with plenty of calcium (dairy products such as milk). Sometimes, despite these efforts, medicine may be needed. All Canadians should take a vitamin D supplement (1,000 – 2,000 IU/day). You may be advised to take calcium supplements. As well, your healthcare provider may recommend bone enhancing medication or hormone replacement therapy.
Some complementary and alternative medicines may possibly help with the symptoms of liver disease, but many can damage the liver. More research is needed in order to assess the role of complementary and alternative medicine in liver disease. Please discuss the use of these therapies with your healthcare provider.
What lifestyle changes may be helpful for PBC patients?
The prognosis of PBC varies greatly from one patient to another. Many lead active lives with few symptoms for more than 10 to 20 years (and even longer). In some patients, however, the condition progresses more rapidly and liver deterioration may occur in just a few years. There is a healthy way to live with a chronic disease and you are encouraged to maintain an active lifestyle under the supervision of your healthcare provider. It is important to know that support is available that may help you improve your quality of life. In consultation with your healthcare provider, you should do your best to:
- Maintain a healthy lifestyle
- Reduce stress
- Be physically active
Resources
Primary biliary cholangitis (PBC) 
Living with your diagnosis
The European Association for the Study of the Liver (EASL) is a major European Association with international influence, dedicated to the study of the liver and liver disease. A group of international PBC patient groups worked together to create this guide to help patients diagnosed with primary biliary cholangitis (PBC) understand the EASL clinical guidelines for this condition, and to demonstrate the importance of a structured, life-long and personalised approach to their care.
Support
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a peer supporter in your area, or would like to join the peer support network, please call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST or email us.
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.



