Variceal Bleeding
Variceal Bleeding and its Management:
Endoscopic and Medical Therapy and Shunt Procedures
What are varices?
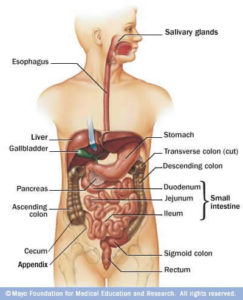
Normally, blood from the intestines and spleen is brought to the liver via the portal vein. In people with severe liver scarring (cirrhosis), however, the normal flow of blood through the liver may become impaired. Blood from the intestines may then be re-routed around the liver through small vessels primarily in the stomach and esophagus.
Some of these blood vessels may become quite large and swollen; they are known as varices. The spleen may also become enlarged in this situation. Varices can occur anywhere within the gastrointestinal tract but occur most commonly in the esophagus and stomach. Due to high pressure (portal hypertension) and thinning of the walls of varices, they may rupture, causing bleeding within the upper gastrointestinal tract. Similarly, sometimes smaller superficial blood vessels become swollen within the lining of the gastrointestinal tract and can occasionally ooze blood. This is referred to as portal hypertensive gastropathy (if in the stomach) or colopathy (if in the colon).
How are varices managed?
In patients with large esophageal or gastric varices that are at risk of rupture, preventive treatment with beta blockers (e.g. nadolol or propranolol) is usually instituted. Beta-blockers reduce the pressure within varices to help prevent their rupture. In some cases, endoscopic therapy (i.e. variceal banding may be instituted to prevent variceal hemorrhage (see below).
Patients with esophageal and/or gastric variceal bleeding require urgent hospital admission. Treatment typically consists of intravenous fluids, and in some cases, transfusion of red blood cells to support the blood pressure. In patients with abnormalities of the blood clotting system, transfusion of platelets and/or clotting factors (e.g. fresh frozen plasma) may be necessary. To help stop bleeding from varices, an intravenous medication called octreotide is typically used. Like beta blockers, octreotide reduces the pressure within the portal venous system. In this situation, emergency endoscopic therapy should also be instituted (see below). Finally, all patients with variceal bleeding should receive appropriate antibiotic therapy. Antibiotics reduce the risk of recurrence of bleeding from varices once bleeding is controlled, prevent infections, and help reduce mortality in these patients.
What is endoscopic therapy?
Endoscopic therapy is a way of preventing and treating variceal bleeding without the requirement for surgery. In the most common procedure called endoscopic variceal banding (or ligation), rubber bands are placed around varices in the esophagus through a flexible endoscope which is used to visualize the vessels. In rare circumstances, if bleeding cannot be controlled by variceal banding, another technique called endoscopic sclerotherapy may be employed. This procedure, which is rarely used currently, involves the injection of diluted mixtures of sclerosing (hardening) solutions into the esophageal varices to lead to their eradication. In the case of varices in the stomach (gastric varices) banding is not usually possible. The preferred management of gastric varices that require therapy is the injection of glue (e.g. histacryl), also at the time of endoscopy.
What are the benefits of endoscopic therapy?
The major benefits of endoscopic therapy are that it is safe and easy to apply. It can be performed at most hospitals and is often done as an outpatient procedure. It is commonly used in the management of patients with cirrhosis and variceal bleeding. It can be used to either prevent varices from rupturing (prophylactic treatment) or as a treatment for bleeding varices. It usually takes more than one session to eradicate esophageal varices, hence repeat endoscopies are often required.
What is a portosystemic shunt?
In cases where severe bleeding occurs and other treatments have failed or are not possible, radiologic or surgical portosystemic shunt procedures may be used to reduce the flow of blood through the varices, reduce pressure within them, and to stop their bleeding. The most commonly employed procedure today is a transjugular intrahepatic portosystemic shunt (TIPS), which is a non-surgical procedure performed by radiologists (see below). In rare circumstances, a surgical shunt may be necessary. This procedure involves the surgical joining of two veins, the portal vein and the inferior vena cava, to relieve pressure in the portal vein that carries blood into the liver. Different types of surgical shunts can be performed; however, they are rarely required today.
What is a transjugular intrahepatic portal-systemic shunt (TIPS)?
A TIPS is a non-surgical shunt which has improved the management of difficult to control portal hypertension. In the case of life-threatening bleeding that cannot be controlled by endoscopic and medical therapy, TIPS is a useful option. TIPS insertion is performed in the x-ray department by radiologists. In this procedure, a needle is inserted via the jugular vein in the neck, advanced into a hepatic vein (which drains blood from the liver), and then into a large branch of the portal vein (which supplies blood to the liver). Using an inflatable balloon-tipped catheter tube, the section between the portal vein branch and the hepatic vein is widened and then kept open (stented) with a cylindrical wire-mesh stent. This shunt serves to bypass blood around the high-pressure blood vessels within the scarred cirrhotic liver, and thereby reduces pressure within the portal veins and branches (including varices).
What are the advantages and disadvantages of TIPS?
The major advantage of TIPS is that it is not a surgical procedure and does not require the use of a general anesthetic, both of which are often poorly tolerated by patients with cirrhosis. Another advantage of TIPS is that it can help reduce the accumulation of fluid in the abdomen (ascites) or around the lungs (pleural effusions) in cirrhotic patients with fluid retention. TIPS have been used successfully to treat severe ascites that no longer responds to the drugs (diuretic) or in patients who have side effects of these drugs. Approximately one-quarter of patients may develop encephalopathy (altered thinking) following insertion of a TIPS. This is usually easily managed with appropriate medication. In addition, these shunts can narrow or become blocked, and therefore need to be monitored regularly by ultrasound. If they do narrow or become blocked, they can usually be opened up with a balloon or the addition of another stent.
Support
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a peer supporter in your area, or would like to join the peer support network, please call the National Help Line at 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST or email us.
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.



