Fatty Liver Disease
Fat in the liver typically develops when a person consumes more fat and sugars than his or her body can handle. This is more common in people who are overweight or obese but can also occur in adults with healthy body weights. If fat builds up to more than 5% of the liver, then the liver is considered to be a fatty liver. Although having this condition may not cause any immediate harm, there is a concern that extra fat in the liver might make the liver vulnerable to further injury such as inflammation and scarring.
Non-alcoholic fatty liver disease (NAFLD) is a liver disease affecting people who drink little to no alcohol. As the name implies, the main characteristics of NAFLD is too much fat stored in liver cells. NAFLD is the most common liver disease in Canada affecting about 20% of Canadians.
It tends to develop in people who are overweight or obese, particularly if they have lot of fat around the middle of their body (waist). It can also develop in a person whose body weight is in the healthy weight range, but who typically eats a lot of sugary and fatty foods and who has extra fat around the waist. NAFLD has shown to be strongly associated with metabolic syndrome—a health disorder characterized by a group of risk factors (large waist circumference, high blood pressure, high blood sugar levels, high cholesterol, and abnormal amounts of lipids in the blood) that greatly increase the risk of many chronic illnesses.
The most common cause of fatty liver disease in Canada is obesity. In 2018, almost 30% of Canadians 18 and older (roughly 7.3 million adults) reported height and weight that classified them as either overweight or obese.
Besides obesity, nutritional causes of fatty liver disease are:
Certain conditions often accompany and may contribute to fatty liver disease:
Other causes include:
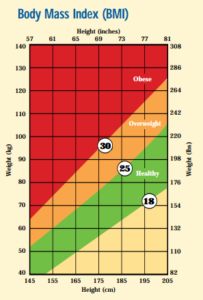 Although many people feel they could lose some weight, few would consider themselves obese. A widely-used measure to define “overweight” and “obese” is the Body Mass Index (BMI). A BMI is a calculation based on your height and weight that gives a number that reflects either a healthy or unhealthy weight.
Although many people feel they could lose some weight, few would consider themselves obese. A widely-used measure to define “overweight” and “obese” is the Body Mass Index (BMI). A BMI is a calculation based on your height and weight that gives a number that reflects either a healthy or unhealthy weight.
You can use the following formula to calculate your BMI:
| BMI: | Weight in kg ________________ (Height in meters)2 |
Example: For someone who is 1.70 meters tall who weighs 80 kilograms…
BMI = 80 ÷ (1.70 x 1.70) = 27.7
Click here to access the BMI Calculator.
Note: Different ethnic groups may differ slightly. For example, in Asian populations the healthy BMI is lower, ranging from 18 – 23.
It is important to note that the BMI is an indirect measure of body fat. It does not take into account muscle mass, bone density, overall body composition, and racial and sex differences.

Excess abdominal fat is associated with fatty liver disease and other health risks such as diabetes. Waist measurements−which differ according to gender—are used to identify the health risks associated with excess abdominal fat.
It is important to measure your waist circumference in a consistent way. The best way to do this is:
Fat and sugars from a person’s diet are usually broken down by the liver and other tissues. If the amount of fat or simple sugar intake exceeds what is required by the body, fat is stored in the fatty tissue. Other reasons for the accumulation of fat in the liver could be the transfer of fat from other parts of the body or the inability of the liver to change it into a form that can be eliminated.
In general, people with fatty liver disease have no symptoms. However, some people report discomfort in the abdomen at the level of the liver, fatigue, a general feeling of being unwell, and vague discomfort.
Fatty liver disease is usually suspected in people who are overweight and obese (particularly those with large waist circumferences), who have evidence of dyslipidemia (high cholesterol and lipids in the blood), insulin resistance and/or abnormal liver tests.
An ultrasound or Fibroscan® of the liver can show the presence of a fatty liver. In some cases, your doctor may advise a liver biopsy, a procedure where the physician inserts a needle into the liver and extracts sample tissue, which is then examined under a microscope.
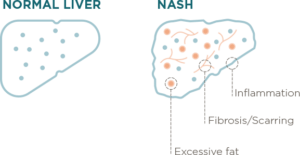
NASH stands for non-alcoholic steatohepatitis and is the more serious form of NAFLD. NASH affects almost 1.5 million Canadians, even those who drink little or no alcohol. Not only can NASH cause liver scarring, called fibrosis, but about 1 out of 5 adults with NASH can develop potential damage to liver function called cirrhosis.
NASH patients are also at greater risk of liver cancer, and for about 1 out of 10 people with NASH, it may lead to liver failure and the need for a liver transplant.
While a simple fatty liver is a rather benign condition, NASH is often associated with ongoing liver damage and can lead to cirrhosis of the liver, liver cancer, and the need for a liver transplant.
As with NAFLD, people with NASH generally have limited symptoms. Although rare, some children may present with vomiting and tenderness of an enlarged liver.
Currently, the long-term outlook of people with NASH is not well understood. In most cases, NASH seems to be a slowly progressive disease. However, there is a small proportion of NASH patients whose cirrhosis will become more severe, possibly leading to liver cancer or liver failure. In chronic liver failure, a liver transplant may be needed.
When there is a buildup of simple fat, the liver becomes vulnerable to further injury, which may result in liver inflammation and scarring. The treatment of fatty liver disease is related to the cause. At this time, it is not possible to predict which patients will develop NASH.
Optimal treatment for NAFLD and NASH has not yet been established. People are advised to address their risk factors (i.e., to improve their blood sugar control/monitoring if they are diabetic and to achieve gradual and sustained weight loss).
It is usually recommended that those diagnosed with NASH should avoid drinking alcohol. Lifestyle modification and excellent control of other illnesses are important for all patients with NAFLD and NASH.
Currently, there is no proven treatment with medication for NAFLD and NASH. Since it is now such a common health condition, NASH has raised much interest in the scientific community. There are numerous clinical trials for various treatments of NASH and several promising drug therapies that are anticipated to pave the way for new and more effective treatment options.
Fatty liver disease is now becoming evident in children, due in large part to an alarming increase in childhood obesity. Currently:
In childhood, a fatty liver can be caused by a variety of disorders including those related to problems with copper metabolism (e.g., Wilson Disease), viral hepatitis, or a variety of autoimmune diseases. It is very important that your doctor makes sure that your child does not have these conditions first.
NAFLD can only be diagnosed in children after all other potential causes of fatty liver have been ruled out. If your doctor or healthcare provider thinks your child may be at risk for NAFLD, they may order some blood tests and an ultrasound of the abdomen to determine whether your child has NAFLD or not. Consult your doctor about what types of tests your child needs to undergo to determine if your child has NAFLD.
When it comes to children, measuring waist circumference and your child’s height can help you determine if your child is depositing extra fat around the middle of their body. It is important to measure your child’s waist circumference, in the same way, each time it is done.
The exact number that you get for a child’s waist circumference is not what is important, as each child grows at different rates and so each child may have a different number. A general rule of thumb is to measure the ratio between your child’s waist circumference and their height (in centimetres). A ratio greater than 0.5 may mean that the child is depositing a little extra fat around their middle. However, it does NOT mean your child has NAFLD.
Waist-to-height ratio = WC (cm)
Height (cm)
The best tool to decide if your child’s body weight is in the healthy range is to plot your child’s weight and body mass index (BMI) on growth curves. A healthy body weight is when your child’s weight or BMI falls between the third percentile and the 95th percentile. If your child’s BMI is above the 95th percentile then your child is obese. If your child’s BMI is between the 85th percentile and 95th percentile, they may be overweight.
It is important to follow the ‘trend’ of where your child is ‘tracking’ on the growth curve and not just one point in time. Remember your child is growing and so you should expect that your child’s BMI will change with time.
BMI is calculated exactly like adults. Your child’s weight (in kg) divided by your child’s height (in meters) squared.
By adopting a healthy lifestyle, you may prevent obesity – the number one reason for fatty liver disease. It is important to remember that a healthy diet and exercise are important components of any weight-loss regimen.
Incorporating these easy everyday tips on nutrition, daily activity, exercise and sleep can help decrease your risk of NAFLD and NASH and increase your chances of feeling more energized and less stressed.
A change in diet plays a significant part in how NAFLD may be treated and certainly how it can be prevented. Consuming too much sugar and saturated fat in your diet can have a similar effect as too much alcohol—fat build-up in the liver. Although there is no specific ‘liver healthy diet,’ these general guidelines of what and how much to eat can help ensure that your liver is functioning at its best!
Added Sugar
The World Health Organization (WHO) guideline recommends adults and children reduce their daily intake of added sugars to less than 10% of their total energy intake. That’s less than 50 grams of added sugars per day!* Learn more (English or French).
Recognizing the difference between physical activity and exercise is the first step to living a lifestyle filled with more movement! While exercise is something best done with a moderate to high intensity and a structured routine, the goal of physical activity is do anything you can that gets you moving and can be physically demanding. It is important to decrease your sedentary activity time. Here are some tips to decrease your time spent in sedentary activity and become more active!
Remember: Make sure you and your loved one stay hydrated, even during physical activities. Carrying a water bottle during any physical activity is recommended.
Heading home after a long day, most of us would just like to rest, relax and rid ourselves of stress. The last thing on the mind may be getting some exercise. But did you know that eating a ton of fatty or sugary foods and not getting enough physical activity puts stress on your liver? To continue reading click here.
Click here to access the Canadian 24-Hour Movement Guidelines for Children, Youth, Adults and Older Adults.
If you were to weigh how important sleep is to your liver health, how far high up or down would it fall on the list? Sleep affects so many parts of life like our mental health, and it should be valued just as much as eating right and getting enough physical activity throughout the day. Many Canadians do not get enough sleep, and the impact can be seen on their liver health.
Sleep and your liver health
Insufficient sleep has been linked to a number of poor physical and mental health concerns, including an increased risk for developing a fatty liver. Lack of sleep can contribute to changes in your overall metabolism (like insulin resistance) that may affect the way your liver converts nutrients from the foods you eat, making it harder to maintain a healthy body weight. It can also make you feel more tired and sleepy during the day which also affects your overall physical activity level.
Health Canada recommends that getting at least 7-9 hours of sleep per night for adults is essential to maintain your health. Children need even more sleep time. Current guidelines recommend 9–11 hours of sleep per night for children ages 5–13 years old, and. 8–10 hours of sleep per night for children 14–17 years old.
Sleeping the recommended hours isn’t the only recipe for obtaining a healthy ‘sleep routine.’ It is also important to maintain a good pattern of sleep without interruptions that may prevent you from getting a good rest.
Sleep Apnea
Lack of sleep can be due to a condition called sleep apnea. If you snore loudly and feel tired even after a full night’s sleep, you might have sleep apnea. One of the most common types of sleep apnea is obstructive sleep apnea, caused by your throat muscles relaxing and affecting the way air enters your lungs.
Common signs and symptoms of sleep apnea include snoring while sleeping, waking up gasping for air several times a night, morning headache, irritability and feeling sleepy during the day. If you think you may have any of these symptoms, speak to your doctor or health care provider.
Canadian Liver Foundation presents webinar: What is Fatty Liver Disease
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a peer supporter in your area, or would like to join the peer support network, please call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST or email us.
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.
© 2024 Canadian Liver Foundation. All rights reserved. Charitable Registration # 10686 2949 RR0001.

Be part of every way we help Canadians with liver diseases - today and in the future. Give this holiday season to fund research, education, prevention and support. 🫶🎁
Sign up for our newsletter and stay up to date on the latest news, updates and resources for liver disease.