Cirrhosis
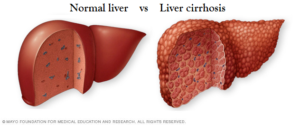
Cirrhosis is a condition (not a disease) that results from permanent damage or scarring of the liver. There are many things that can cause damage to the liver, such as too much fat or alcohol, as well as conditions related to infections, genes, and the immune system. This affects the liver from performing its many functions.
Used with permission from Cirrhosis Care Alberta. For more information, visit www.cirrhosiscare.ca
When something damages the liver, scar tissue begins to form. This scarring is called fibrosis. It happens little by little over many years. When the entire liver is scarred, it shrinks and gets hard. This is called cirrhosis. Any illness that damages the liver may lead to fibrosis and, eventually, cirrhosis.
A liver with cirrhosis can have a harder time getting all its factory work done. This prevents the liver from making the good substances it normally makes, such as blood clotting factors and albumin. Albumin is a protein with lots of important functions. A liver with cirrhosis also has trouble sorting out what your body needs, like sugar and vitamins, and what it does not need, like toxins and bacteria. Some people may even experience intense itching due to products that are deposited in the skin. Liver cancer can also develop in a liver with cirrhosis.
Causes
Cirrhosis can have many causes. Some of the main ones include:
- Viral infections caused by chronic viral hepatitis (such as hepatitis B & hepatitis C).
- Long-term, heavy use of alcohol.
- Non-alcoholic fatty liver disease (NAFLD) & non-alcoholic steatohepatitis (NASH).
- Biliary tract diseases, such as primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC).
- Inherited diseases, such as Wilson disease and hemochromatosis.
- Toxic hepatitis caused by severe reactions to prescription drugs or prolonged exposure to environmental toxins.
- Metabolic disease, such as alpha-1-antitrypsin deficiency, galactosemia and glycogen storage disorders.
- Repeated bouts of heart failure with liver congestions.
- Biliary atresia, a condition caused by absent or injured bile ducts, is the most common cause of cirrhosis in babies. These babies are jaundiced after their first month of life due to a build-up of bile in the liver. New ducts can be surgically formed in some cases restoring normal bile secretion. Transplantation is required in other cases.
Diagnosis & Treatment
If you suspect you have cirrhosis, make an appointment with your healthcare provider. Only a healthcare provider can confirm if you have cirrhosis.
There are many signs of cirrhosis that your healthcare provider may find during a physical exam. You may have red palms or small spider-like veins on your face or body. You may also have fluid buildup in your abdomen, called ascites.
Your healthcare provider might order blood tests as well as other types of tests that can give your provider a good idea of whether you have cirrhosis. These tests can include an ultrasound, CT scan, MRI or a radioisotope liver/spleen scan. There is also a special kind of ultrasound (such as Fibroscan®) that measures the amount of stiffness in your liver (as the liver gets scarred, it gets stiffer.) You may also be asked to have a liver biopsy. A liver biopsy shows how much scarring is in your liver. It can help your healthcare provider figure out what is causing the damage and how best to treat it. Once it is determined that liver disease is present, immediate treatment is recommended.
What is Portal Hypertension?
A healthy liver is soft, like a sponge. It gets most of its blood supply from a large blood vessel called the portal vein.
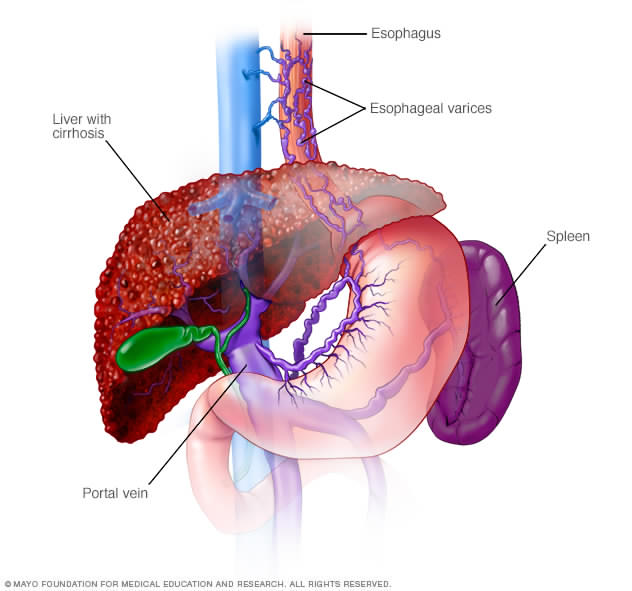
When the liver is soft, blood can flow into it easily, like water from a hose pouring into a sponge. Imagine that sponge gets hard like a rock. Water from the hose cannot flow in as easily and pressure builds up in the hose. Just like the hose, pressure in the portal vein can build up when the liver becomes hard, and blood cannot flow into it very well. This condition is called portal hypertension.
To relieve pressure in the portal vein, the blood takes detours around the liver in other veins. Some of these veins are in the esophagus, the tube that carries food from your mouth to your stomach. Other veins are in the stomach itself. Some of these new blood vessels, called varices, which can form in the stomach and esophagus, become large and may rupture due to the high blood pressure and thin vessel walls, causing bleeding in the upper stomach or esophagus.
Portal hypertension can also make your spleen bigger. One of the jobs of the spleen is to control the number of platelets you have in your body. Platelets help your blood to clot. When the spleen gets bigger and cannot do its job properly, you may notice you bruise more easily, or it takes longer to stop bleeding if you hurt yourself. Portal hypertension is important, because it can lead to major complications of cirrhosis, such as ascites and varices.
Treatment
Treatments for cirrhosis are aimed at stopping or delaying the disease progression (worsening of disease), minimizing liver cell damage, and reducing complications. For example, when cirrhosis is caused by alcohol, it is essential to stop drinking to stop the progression of the disease. For most other causes of cirrhosis, cessation of alcohol is also generally recommended. Cirrhosis caused by viral hepatitis (Hepatitis B & Hepatitis C) may be treated with antiviral drugs to reduce injury to liver cells.
Medications can also be given to control the symptoms of cirrhosis. For instance, drugs called diuretics are used to remove excess fluid and to prevent edema (swelling) and ascites from recurring. However, a low salt diet is also essential to treat those with ascites. Drug therapy can also improve altered mental function associated with cirrhosis. Laxatives may be given to help absorb toxins and speed their removal from the intestines. A serious consequence of cirrhosis may be bleeding as a result of portal hypertension. Medications, such as beta blockers, may be prescribed to reduce portal hypertension.
Even when complications develop, they can usually be treated. If the patient bleeds from the varices of the stomach or esophagus, the doctor can place rubber bands around these veins through a flexible tube (endoscope) that is inserted through the mouth and esophagus. Occasionally these veins are injected with a sclerosing (hardening) agent to stop bleeding. In critical cases, a portacaval shunt (which relieves the pressure in the portal vein and varices) or a liver transplant may be necessary.
Stages of Cirrhosis
Cirrhosis can be divided into 2 stages, Compensated Cirrhosis and Decompensated Cirrhosis.
For most people, cirrhosis progresses (or gets worse) over time, but if the main cause of cirrhosis is treated, such as eliminating hepatitis C or quitting alcohol, it can help a lot.
Cirrhosis can shorten the length of a person’s life, but in many cases does not. The only cure for cirrhosis is liver transplant. It is important to understand that liver transplant is a major surgery with many potential risks and is not recommended for everyone with cirrhosis. No matter what stage your cirrhosis is at, your healthcare team will work with you to manage any symptoms or major complications that you have.
Compensated Cirrhosis
At first, you may have no symptoms at all. This is called compensated cirrhosis. People with compensated cirrhosis may live many years without being aware that their liver is scarred. This is because the pressure in the portal vein is not yet too high, and there are still enough healthy liver cells to keep up with the body’s needs. In other words, although the liver is very scarred, it is still able to do its jobs.
But if the cirrhosis is not diagnosed and treated, the pressure in your portal vein gets higher. The few remaining healthy liver cells get overwhelmed. Then you may notice symptoms like:
- low energy
- poor appetite
- weight and muscle loss
- depressed mood
- itching
- loss of sexual function
Decompensated Cirrhosis
As cirrhosis progresses even more, you can develop major complications. These can be related to portal hypertension or because the liver cannot do its jobs as well as it did before.
The most common major complications are:
- fluid build-up in your abdomen (ascites) or chest (called pleural effusion)
- bleeding inside your body from the swollen veins (called variceal bleeding), and
- confusion related to the cirrhosis (called hepatic encephalopathy)
- People with advanced cirrhosis have trouble removing toxins effectively, leading to toxin accumulation in the blood, which in turn can impair mental function and lead to personality changes and possibly coma. Early signs of toxin accumulation in the brain may include neglect of personal appearance, unresponsiveness, forgetfulness, concentration problems or changes in sleeping habits. Because the normal cleansing process is impaired by cirrhosis, drugs are not properly filtered resulting in an increased sensitivity to drugs and their side-effects.
Other complications in the later stages of cirrhosis include:
- Jaundice (yellowing of the skin and the whites of the eyes)
- Gallstones (because of the insufficient levels of bile – the digestive fluid produced by the liver – that reaches the gallbladder)
When you have developed any of these major complications, it is called decompensated cirrhosis.
Having decompensated cirrhosis is a sign that you will need to work closely with your healthcare team to manage your symptoms and major complications. Your healthcare team may also suggest you be assessed for a liver transplant.
Living with Cirrhosis
Eating Well with Cirrhosis
Cirrhosis Resource Library
 This Guide covers general topics relevant to all patients with cirrhosis. Specific nutrition issues are also addressed that may be helpful at other times. The Guide is a tool for use throughout your cirrhosis journey. It also includes recipes that are suitable for all individuals and can be modified to accommodate food allergies, dietary restrictions, and preferences.
This Guide covers general topics relevant to all patients with cirrhosis. Specific nutrition issues are also addressed that may be helpful at other times. The Guide is a tool for use throughout your cirrhosis journey. It also includes recipes that are suitable for all individuals and can be modified to accommodate food allergies, dietary restrictions, and preferences.
This patient information toolkit is designed to help patients gain a better understanding of their condition so they can make the best decisions for treatment and health. This toolkit outlines general information on cirrhosis, complications, treatments, as well as an ascites tracker, hepatic encephalopathy tracker, and alcohol and substance abuse resources.
 One of the Canadian Liver Foundation’s research partners, Cirrhosis Care Alberta (CCAB), developed an educational website containing helpful information for cirrhosis patients, their families, and healthcare professionals. For more information, please visit www.cirrhosiscare.ca
One of the Canadian Liver Foundation’s research partners, Cirrhosis Care Alberta (CCAB), developed an educational website containing helpful information for cirrhosis patients, their families, and healthcare professionals. For more information, please visit www.cirrhosiscare.ca
Support
National Help Line:
This support resource gives you and your loved one somewhere to turn for answers after diagnosis, helps you understand your disease, and provides you with the resources you need. You can call 1 (800) 563-5483 Monday to Friday from 9 AM to 5 PM EST.
The National Peer Support Network:
This is a national network of people living with liver disease that have offered to share their experiences with others. It was developed by the Canadian Liver Foundation as a means to link Canadians like you who have a family member who has liver disease, who care for someone who suffers from liver disease, or who have been diagnosed with a liver disease, to talk about your concerns with a peer in a similar situation.
If you would like to be connected with a Peer Supporter in your area, or would like to join the National Peer Support Network, please fill out the National Peer Support Network Sign-up Form.
Help us help you!
If you are not satisfied with the information you just read or any information on our website, please take a moment to send us your comments and suggestions on the type of content you would like to find on liver.ca. Please include the page you are commenting about in the subject line of your email.